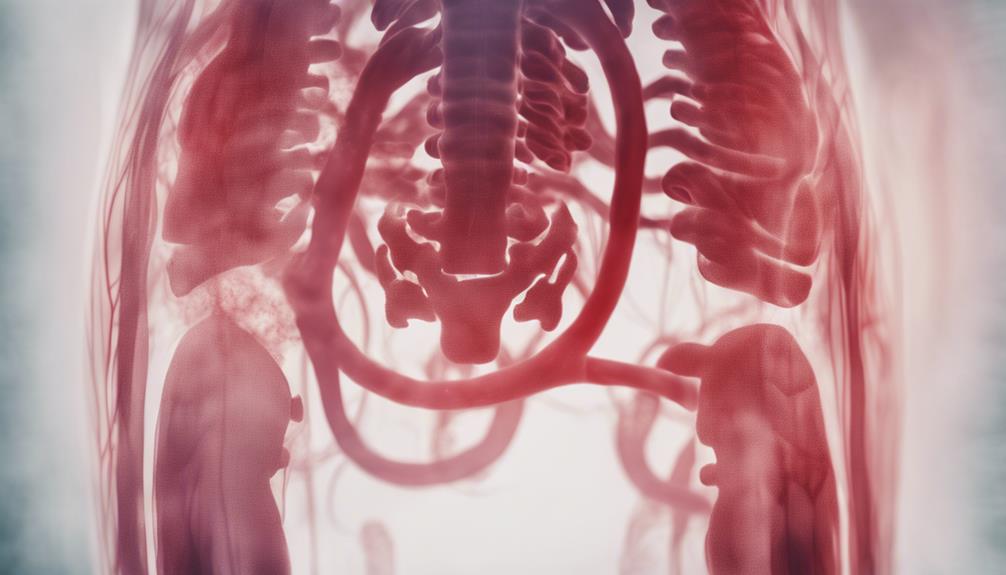
You're likely searching for answers about hemoperitoneum, a life-threatening condition characterized by bleeding into the abdominal cavity. Causes range from ruptured intraabdominal vessels and trauma to medical conditions like ectopic pregnancies and visceral artery lesions. Diagnostic challenges arise from radiological imaging limitations, such as CT scan sensitivity ranging from 60-70%. Symptoms vary widely, from mild discomfort to severe instability, and delayed diagnosis can lead to significant morbidity and mortality. Thorough history-taking, physical examination, and imaging are essential for accurate diagnosis. As you explore this complex condition, you'll discover the importance of prompt intervention and the various treatment options available.
Key Takeaways
- Hemoperitoneum is a life-threatening condition characterized by bleeding into the abdominal cavity, often resulting from trauma, ruptured vessels, or medical conditions.
- Prompt diagnosis is crucial, as delayed diagnosis can lead to significant morbidity and mortality, and imaging techniques like CT scans, ultrasound, and angiography can aid in diagnosis.
- Clinical presentation varies widely, ranging from mild discomfort to severe instability, and may include abdominal pain, hemodynamic instability, and uncontrolled hypertension.
- Treatment options include surgical intervention, such as laparotomy and endovascular embolization, as well as conservative care methods, which focus on close monitoring and early intervention.
- Early diagnosis and intervention are critical, as hemoperitoneum can lead to severe complications, including hemorrhagic shock, peritonitis, and organ dysfunction, if left untreated.
Causes of Hemoperitoneum
When identifying the underlying causes of hemoperitoneum, it's important to consider a range of factors, such as ruptured intraabdominal vessels, trauma, and various medical conditions. As you investigate further, you'll discover that spontaneous hemoperitoneum can occur due to bleeding from abdominal blood vessels, which can be idiopathic or linked to underlying conditions.
Ruptured ectopic pregnancies, ovarian cysts, and retrograde menstruation are common gynecologic causes of hemoperitoneum. Additionally, vasculitis, anticoagulant therapy, hepatic metastases, and visceral artery lesions can also contribute to this condition.
In an emergency situation, prompt management is crucial to prevent further bleeding and peritoneal fluid accumulation. It's important to recognize the signs and symptoms of hemoperitoneum to provide timely intervention. By understanding the causes of hemoperitoneum, you'll be better equipped to handle this medical emergency and improve patient outcomes.
Diagnostic Challenges
As you navigate the complexities of hemoperitoneum, you'll encounter diagnostic challenges that can hinder accurate diagnosis. Radiological imaging limitations can make it difficult to distinguish between ascites and hemorrhage, while variability in clinical presentation can lead to misdiagnosis.
You'll need to ponder these challenges carefully to guarantee timely and effective treatment interventions.
Radiological Imaging Limitations
Radiological imaging's limited sensitivity poses significant diagnostic challenges in pinpointing the bleeding origin in hemoperitoneum cases, often leaving you with more questions than answers. Despite advancements in imaging technology, the elusive nature of idiopathic spontaneous hemoperitoneum can still present diagnostic hurdles for healthcare providers.
| Imaging Modality | Sensitivity | Diagnostic Challenges |
|---|---|---|
| CT Scan | 60-70% | Difficulty in identifying small bleeding sources |
| Ultrasound | 50-60% | Limited visibility in obese patients |
| MRI | 70-80% | Higher cost and limited availability |
| Angiography | 80-90% | Invasive procedure with potential complications |
| PET Scan | 40-50% | Limited resolution and high cost |
The table above highlights the limitations of various radiological imaging modalities in identifying the source of bleeding in hemoperitoneum cases. The lack of specific radiological findings can complicate the diagnosis and management of idiopathic spontaneous hemoperitoneum. In some cases, radiological imaging may not provide a definitive answer regarding the underlying cause of hemoperitoneum, necessitating further evaluation. As a result, healthcare providers must rely on a combination of clinical evaluation, laboratory tests, and imaging studies to diagnose and manage hemoperitoneum effectively.
Clinical Presentation Variability
You're faced with a diagnostic puzzle when a patient presents with unexplained abdominal pain or signs of shock, as the clinical presentation of hemoperitoneum can vary widely, making it challenging to pinpoint the source of bleeding.
The variability in symptoms, ranging from mild abdominal discomfort to severe hemodynamic instability, adds to the diagnostic challenges. Identifying the source of bleeding can be difficult, especially in cases of idiopathic spontaneous hemoperitoneum where the bleeding origin is unknown.
It's important to bear in mind hemoperitoneum in patients with unexplained abdominal pain or signs of shock, as delayed diagnosis and treatment can lead to significant morbidity and mortality. A thorough history-taking, physical examination, and diagnostic imaging are essential to accurately diagnose hemoperitoneum.
The importance of prompt recognition can't be overstated, as timely intervention can greatly impact patient outcomes. By understanding the variability in clinical presentation, you can better navigate the diagnostic challenges of hemoperitoneum and provide excellent care for your patients.
Imaging Techniques

When evaluating hemoperitoneum, you rely heavily on imaging techniques to pinpoint the source of bleeding and guide timely interventions.
Computed tomography (CT) scans play a pivotal role in confirming intra-abdominal hemorrhage in hemoperitoneum cases.
Abdominal ultrasonography is another valuable tool for identifying the source of bleeding, especially in equivocal cases.
Additionally, RBC scintigraphy can aid in localizing active bleeding sources in patients with hemoperitoneum.
The results of these diagnostic imaging techniques inform radiological intervention decisions, taking into account patient stability and bleeding sources.
Early use of these techniques is essential for prompt diagnosis and intervention in hemoperitoneum cases.
Clinical Presentations

In patients with hemoperitoneum, clinical presentations often manifest as atypical abdominal pain, which can be accompanied by hemodynamic instability, and may even exhibit symptoms of uncontrolled hypertension, increasing the risk of bleeding.
You may experience severe abdominal tenderness, nausea, and vomiting, which can worsen over time.
A 'double-rupture' phenomenon in hemoperitoneum can lead to rapid clinical deterioration, making early diagnosis vital.
If left untreated, hemoperitoneum can lead to hemorrhagic hypovolemic shock, greatly impacting mortality risk.
As a patient, it's important to recognize these symptoms and seek immediate medical attention.
Early diagnosis and intervention are essential in managing hemoperitoneum and improving patient outcomes.
Delayed or misdiagnosis can result in severe consequences, highlighting the importance of accurate clinical presentations.
Treatment and Management

As you explore the treatment and management of hemoperitoneum, you'll find that there are two primary approaches: surgical intervention options and conservative care methods.
You'll need to contemplate the severity of the condition, the patient's overall health, and the source of the bleeding when deciding between these two paths.
Surgical Intervention Options
You have several surgical intervention options to contemplate for treating hemoperitoneum, including laparotomy, laparoscopy, and endovascular procedures. These options are often necessary for patients experiencing active bleeding or unstable crucial signs.
The primary goal of surgical management is to control bleeding, repair damaged vessels or organs, and prevent further hemorrhage. Endovascular embolization, a minimally invasive technique, is particularly effective in stopping bleeding from arterial sources.
Your doctor will consider the underlying cause of hemoperitoneum, your overall stability, and the location of the bleeding source when choosing the most suitable surgical intervention. For instance, laparotomy may be necessary for unstable patients or those with significant bleeding, while laparoscopy may be a better option for more stable patients with less severe bleeding.
Ultimately, the choice of surgical intervention depends on a thorough evaluation of your individual situation. By understanding these surgical options, you can make informed decisions about your care and work effectively with your healthcare team to manage hemoperitoneum.
Conservative Care Methods
During the initial stages of treatment, your healthcare team will likely employ conservative care methods to manage your hemoperitoneum, particularly if you're a stable patient. This non-operative approach focuses on close monitoring and early intervention to guarantee your stability and prevent complications. Conservative management has been shown to result in successful outcomes, especially in cases of idiopathic spontaneous hemoperitoneum.
| Components of Conservative Care | Purpose | Benefits |
|---|---|---|
| Close Monitoring | Identify potential complications | Facilitates early intervention |
| Fluid Resuscitation | Restore blood volume | Prevents shock and organ failure |
| Transfusions | Replace lost blood | Maintains oxygen delivery to organs |
| Observation | Monitor patient's condition | Allows for prompt intervention if needed |
| Early Intervention | Prevent complications | Reduces morbidity and mortality |
Your healthcare team will work closely with you to develop a personalized conservative care plan, which may include observation, fluid resuscitation, and transfusions as needed. By taking a conservative approach, you can benefit from essential components of care that prioritize your stability and promote successful outcomes.
Complications and Prognosis

Hemoperitoneum's complications, which can be severe and even life-threatening, include hemorrhagic shock, peritonitis, and organ dysfunction. You may experience hemorrhagic shock, a potentially fatal condition that occurs when you lose too much blood.
Peritonitis, an infection of the lining of the abdominal cavity, can also develop. Additionally, organ dysfunction can occur, leading to further complications. If left untreated, hemoperitoneum can lead to disseminated intravascular coagulation (DIC), a severe bleeding disorder.
Your prognosis varies depending on the underlying cause, but prompt intervention can significantly improve outcomes. Unfortunately, mortality rates can be high if hemoperitoneum isn't promptly diagnosed and managed. Long-term complications may include adhesions, abscess formation, and chronic pain.
It's essential to seek medical attention immediately if you're experiencing symptoms of hemoperitoneum. With prompt intervention, you can reduce the risk of severe complications and improve your prognosis.
Frequently Asked Questions
What Is the Survival Rate for Hemoperitoneum?
You're wondering about the survival rate for hemoperitoneum. According to studies, it varies from 39% to 75%, depending on the underlying cause and how quickly you receive treatment.
How Serious Is a Hemoperitoneum?
"Break out the smelling salts, because you're about to get hit with a serious diagnosis – a hemoperitoneum is extremely serious, potentially life-threatening, and demands immediate medical attention, so don't hesitate, get help pronto!"
How to Fix Hemoperitoneum?
You'll likely need surgery or radiological procedures to fix hemoperitoneum, but in some cases, non-operative management might be enough; it depends on your stability and the source of the bleeding, so your doctor will guide you.
What Is the Most Common Cause of Spontaneous Hemoperitoneum?
You're wondering what's behind spontaneous hemoperitoneum. Well, you should know that retroperitoneal hemorrhage from arterial aneurysms is the most common cause, accounting for a significant number of cases.
Can Hemoperitoneum Cause Any Audio-related Symptoms?
Hemoperitoneum can potentially lead to audio-related symptoms due to its impact on the body. While not a direct result of the condition itself, the discomfort and pain caused by hemoperitoneum may affect an individual’s ability to concentrate and engage in activities, including exploring the process of remuxing.
Conclusion
As you navigate the complex landscape of hemoperitoneum, it's clear that understanding this medical mystery requires a multifaceted approach, like piecing together an intricate puzzle.
By recognizing the diverse causes, diagnostic challenges, and effective imaging techniques, healthcare professionals can provide timely and targeted treatment, ultimately improving patient outcomes and reducing the risk of complications.
By illuminating this complex condition, we can reveal better management strategies and improve the prognosis for those affected.










